Immune Dsyregulation in Classical Monocytes and Platelets
The project is based on discoveries our Center made previously, in which we identified classical monocytes, a component of the innate immune system, as the circulating immune cells that show that strongest dysregulation in gene expression in ME/CFS. We also looked for changes in gene expression across the immune system that might correlate with post-exertional malaise (PEM), using samples collected before exercise and 24 hours later. This approach revealed that PEM after a strenuous exercise challenge results in a distinctive change in platelets. Thus, going forward, our major goals are to comprehensively investigate monocyte and platelet abnormalities in ME/CFS.
Two complementary approaches will be used to examine monocytes in ME/CFS. First, multiomic approaches will comprehensively determine the gene regulatory changes in monocytes that occur in ME/CFS. One possible result from these experiments will be the identification of the key drivers of monocyte dysregulation in ME/CFS. Second, assays will be performed to test whether the illness results in alterations in the ability of monocytes to migrate and differentiate into macrophages, a critical function of monocytes. These assays are motivated by our current data, which suggests that monocytes in ME/CFS are aberrantly primed to enter tissues, which is a normal function of monocytes but may be inappropriately active. The biopsy project led by Dr. Cosgrove will examine this possibility by directly investigating macrophages in muscle. We will be able to examine links between monocyte alterations in the circulation and the possible consequences in tissue.
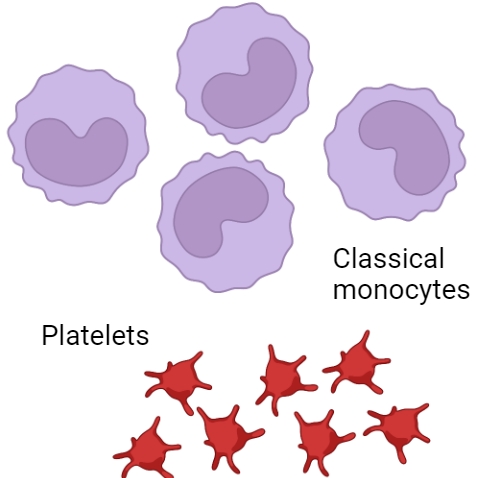 Platelet defects could contribute to circulatory and other symptoms in ME/CFS. Our goal is to examine the platelet transcriptome comprehensively and also to perform assays to test platelet function. We will examine interactions between platelets and other immune cells in ME/CFS that might be contributing to their altered state in the illness. We will also be able to find out whether the cargo of platelet-derived extracellular vesicles is altered in ME/CFS, complementing the analysis of platelets themselves.
Platelet defects could contribute to circulatory and other symptoms in ME/CFS. Our goal is to examine the platelet transcriptome comprehensively and also to perform assays to test platelet function. We will examine interactions between platelets and other immune cells in ME/CFS that might be contributing to their altered state in the illness. We will also be able to find out whether the cargo of platelet-derived extracellular vesicles is altered in ME/CFS, complementing the analysis of platelets themselves.This NIH funded (U54AI178855) project will be led by Dr. Andrew Grimson, an Associate Professor at Cornell University, in collaboration with Dr. Hanson's group and Dr. Dawei Li, an Associate Professor at Texas Tech University Health Sciences Center. Dr. Grimson’s lab will use a combination of genomic and functional assays to investigate components of the immune system in ME/CFS, working closely with Dr. Li, a computational biologist. The genomics assays will be performed in partnership with Dr. Grenier, who leads our Research Core component of the Center.
 Center for Enervating NeuroImmune Disease
Center for Enervating NeuroImmune Disease